October 2024 Monthly Report

In this blog post, we discuss our October 2024 report and provide more information on how to interpret the results. The PDF report can be found at the end.
Key findings:
- The median fentanyl concentration found across all drug categories was 10%
- The median fluorofentanyl concentration found across all drug categories was 6%. Fluorofentanyl adulteration in opioid - down samples has fallen compared to last month.
- Benzodiazepines were found in 34.9% (83/238) of expected Opioid - Down samples
- Bromazolam, the most common benzo found within Opioid - Down samples, was found in 73 Opioid - Down samples with a median concentration of 3% and maximum concentration of 27%
- Xylazine was found in 8.8% (21/238) expected Opioid - Down samples with a median concentration of 0.2% and a maximum concentration of 10%
- Medetomidine was found in 4 expected Opioid - Down samples with a median concentration of 0.8% and a maximum concentration of 1%
Insight for the October 2024 Monthly Report
This blog, and the associated pdf report, breakdown our sample counts into six categories:
- Samples received through direct service provision in Victoria, where service users are bringing samples into the Substance storefront. These samples are labelled as “Substance” samples in the figures/tables of this blog post
- Samples received through direct service provision in Campbell River, where service users bring samples either to the Vancouver Island Mental Health Society (VIHMS) or Campbell River AVI Health & Community Services. These samples are labelled as “Campbell River”
- Samples received through direct service provision in the Comox Valley, where service users are bringing samples to AVI Health & Community Services in Courtenay, BC. These samples are labelled as “Comox Valley”
- Samples received through direct service provision in the Cowichan Valley, where service users bring samples to the Duncan Lookout Society OPS in Duncan, BC. These samples are labelled as “Duncan”
- Samples received through direct service provision in Port Alberni, where service users bring samples into Port Alberni Shelter Society’s OPS. These samples are labelled as “Port Alberni”
- Samples received through direct service provision in Port Hardy, where service users bring samples into Island Health Mental Health and Substance Use. These samples are labelled as “Port Hardy”
- Samples received through indirect service provision, where samples are collected through no-contact drop-off envelopes, are collected by harm reduction workers and other community members at supported housing sites, overdose prevention sites, supervised consumption locations, and the Hospital sample submission kiosks located in Victoria, Nanaimo, and Campbell River. These samples are labelled as “Outreach” samples in the figures/tables herein.
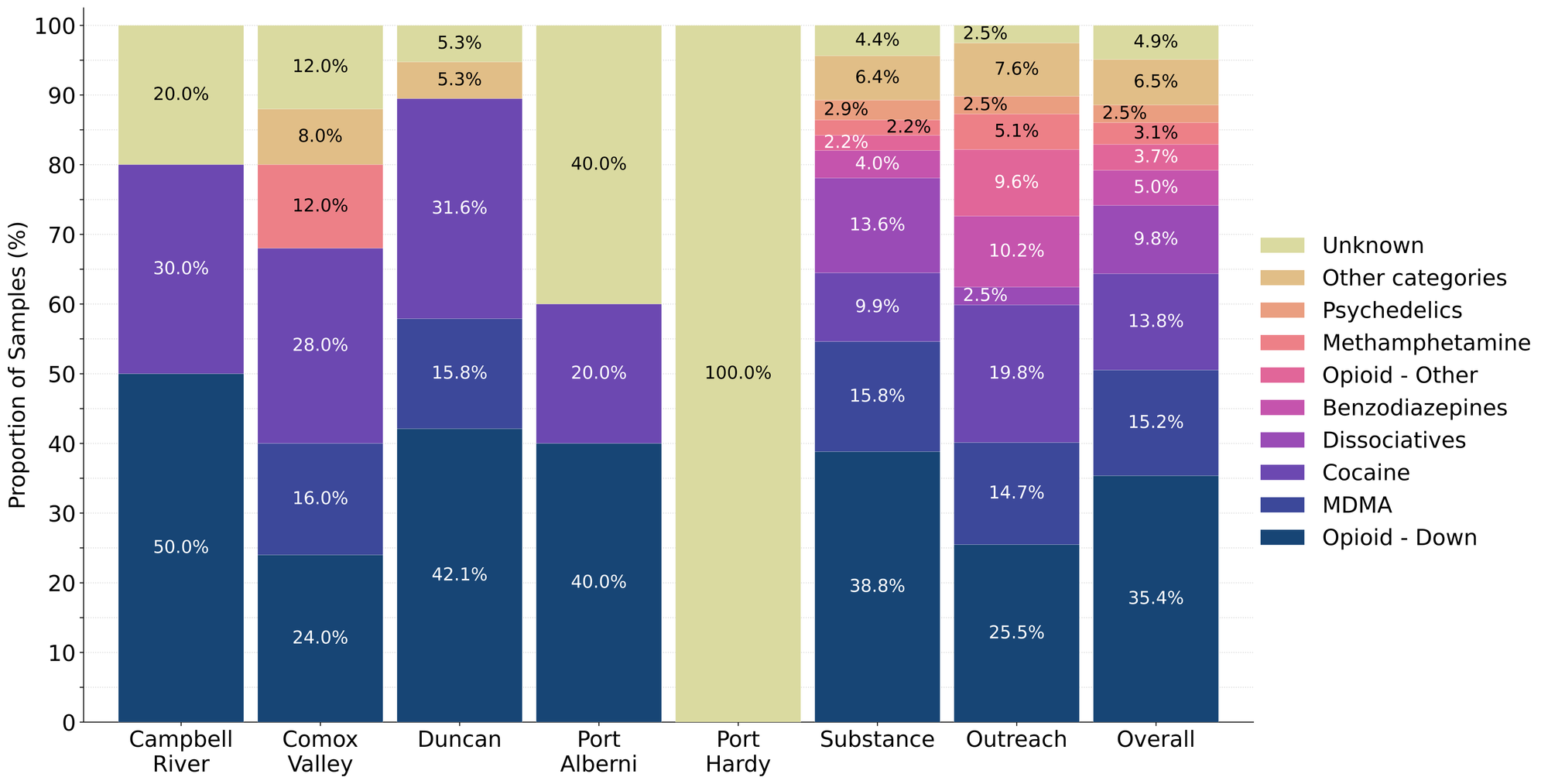
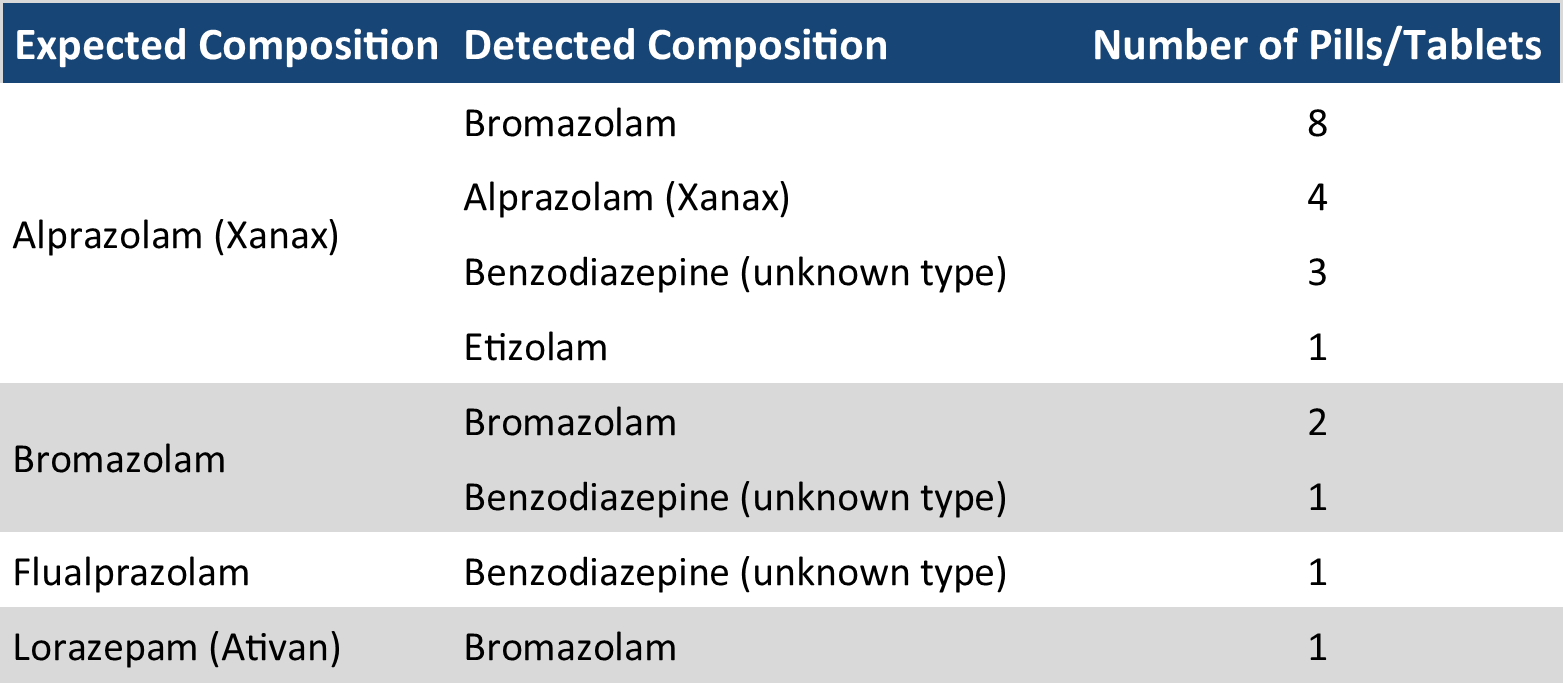
Drug types
Day to day at Substance, we receive and check a wide variety of different samples. Figure 1 shows the prevalence of each expected drug category checked, split by sample collection location/method. Table 1 shows the number of samples received at each sample collection location per expected drug category.
The Sample Breakdown
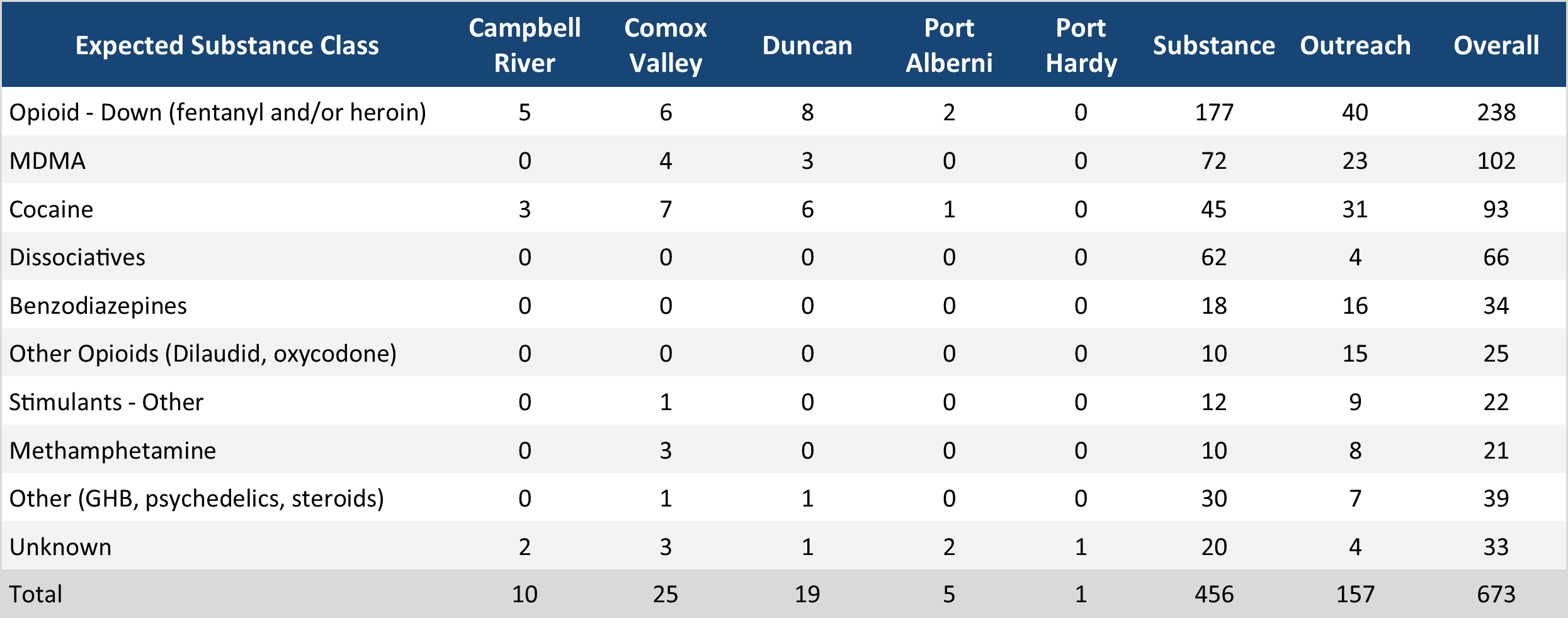
For the majority of samples checked, we confirm the presence of the expected drug with no additional active compounds detected above the limitations of the drug check. The bar charts below highlight a few classes of drugs, differentiating samples where only the expected active component was detected - from situations when other unexpected active components were detected.
Dissociatives
78.8% (52/66) of expected Dissociatives samples (65 ketamine samples, 1 DXM sample) were as expected. The remaining samples were as follows.
13 samples contained an unexpected active component instead of the expected dissociative:
- 1 expected DXM sample (from Victoria) was ketamine instead
- 12 expected ketamine samples (from Victoria) were MDA instead
1 sample contained an active component in addition to the expected dissociative:
- 1 expected ketamine sample also contained MDMA
Cocaine
91.4% (85/93) of expected Cocaine samples (64 cocaine samples, 28 crack samples) were as expected. The remaining samples were as follows.
5 samples contained an active component in addition to cocaine or crack:
- 2 expected crack samples (from Duncan) also contained phenacetin
- 1 expected crack sample (from Port Alberni) also contained ketamine base
- 1 *expected crack sample (from Substance) also contained levamisole
- 1 expected cocaine sample (from Outreach) also contained levamisole
2 expected crack samples (one from Duncan, one from Substance) did not contain active components.
1 expected unspecified cocaine/crack sample (from the Comox Valley) did not contain active components.
Methamphetamine
95.2% (20/21) of expected Methamphetamine samples were as expected. The remaining samples were as follows.
1 sample contained an active component in addition to methamphetamine:
- 1 sample (from Substance) also contained fentanyl
MDMA/MDA
94.1% (96/102) of expected MDMA samples (95 MDMA samples, 5 MDMA and MDA samples, 2 MDA samples) were as expected. The remaining samples were as follows.
3 samples contained an active component in addition to MDMA:
- 1 expected MDMA sample (from the Comox Valley) also contained ketamine
- 2 expected MDMA samples (from
3 expected MDMA samples did not contain any active components
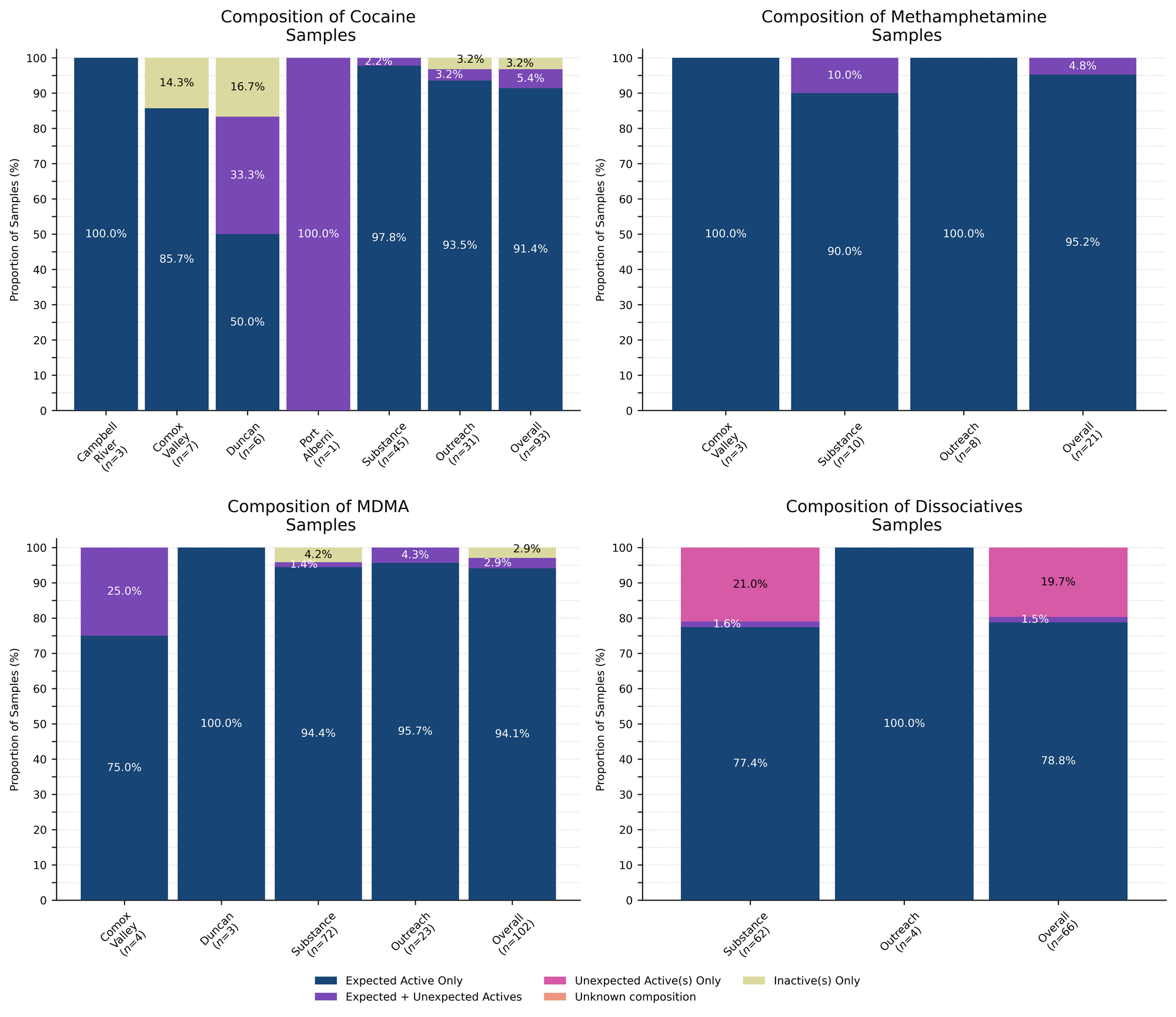
Benzodiazepines (n=28)
61.8% (21/34) of the expected benzodiazepine samples checked in October came to our service sites in the form of pressed pills with the following expected and detected compositions:
Within the remaining 13 samples (all from Victoria):
- 1 expected alprazolam (Xanax) sample was bromazolam instead
- 1 expected alprazolam (Xanax) sample was acetaminophen (Tylenol) instead
- 3 expected Avizafone sample were Avizafone
- 2 expected bromazolam sample was bromazolam
- 1 expected bromazolam sample was bromazolam, fentanyl, and methamphetamine
- 1 expected clonazepam (Klonopin) sample was an unknown benzo instead
- 1 expected unspecified benzo was bromazolam
- 1 expected unspecified benzo was bromazolam and fentanyl
- 2 samples did not contain active components
Opioid-positivity in non-opioid-down samples
In October, we checked 402 samples that were not expected to contain fentanyl or other “unexpected” opioids[1]. Since the opioid-down supply is no longer “just heroin” or “just fentanyl” and is instead a complex, potent, and ever-changing polysubstance market containing other synthetic opioids like fluorofentanyl or nitazenes, here we will examine the prevalence of any unexpected opioid, not just fentanyl, detected in non-opioid-down samples.
Specifically, we are excluding samples that were expected to be “opioid-down” or samples that had an “unknown/missing” expected composition. In the case of “opioid-other” samples, e.g. hydromorphone tablets and oxycodone pills, “unexpected opioids” are defined as any opioid that is not the expected opioid. ↩︎
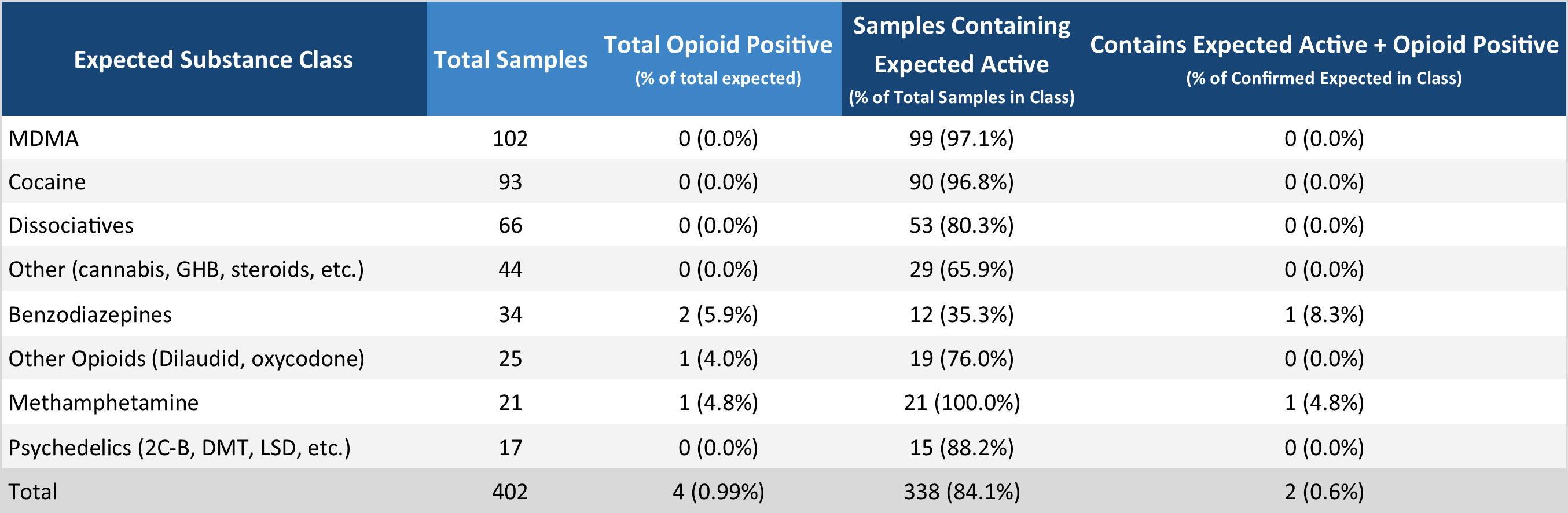
Examining Table 3, we find that 4 samples tested positive for unexpected opioids in October, representing ~1% of all non-opioid-down samples checked. These samples were as follows:
Expected Benzodiazepines samples:
- 1 expected bromazolam sample also contained fentanyl and methamphetamine
- 1 expected unspecified benzo was bromazolam and fentanyl
Expected Methamphetamine samples:
- 1 expected methamphetamine sample also contained fentanyl[1]
Expected Opioid - Other samples:
- 1 expected hydromorphone sample contained isotonitazene instead
In October, no unexpected opioids were detected in samples expected to be MDMA, Cocaine, dissociatives, other, or psychedelics.
In people’s personal quests for bodily autonomy and informed consumption, there is often evaluation of risk and consequence, but when the consequences can be severe and the risks are unknown or are intentionally exaggerated, these become difficult, if not impossible, conversations to weigh. We believe that drug checking can help provide people with the information needed to evaluate the risks, and provides harm reduction advice to minimize undesired consequences of substance use. These data are not meant to downplay concerns or invalidate past experiences. We recognize the tragic consequences of when fentanyl is found in non-opioid samples and honour the heartbreak that such experiences produce. Instead, we present these data with the intent to combat misinformation and provide an evidence-based context for people to consider when making decisions about substance use. While these numbers reflect what we have seen over the course of the project, these (roughly) 1-in-100 events still occur, so we always encourage folks to get their stuff checked.
The presence of fentanyl in these samples is most likely due to cross-contamination with an opioid - down sample. ↩︎
Opioid-Down (n=238)
In this section we present results specific to the opioid-down supply, therefore they may differ from the highlighted findings above that are inclusive of all expected drug categories.
- 56.3% (134/238) of expected opioid-down samples contained fentanyl as the only active opioid
- 5.0% (12/238) of expected opioid-down sample contained fluorofentanyl as the only active opioid
- 11 samples contained heroin, of these samples, 8 contained the related alkaloid acetylcodeine and/or acetylmorphine (MAM). In total, this represents 5% of all opioid - down samples.
- 8/11 samples which contained heroin also contained fentanyl or a fentanyl analogue
- 1 sample contained carfentanil
- 27.3% (65/238) of expected opioid - down samples contained ortho-methyl fentanyl
- 34.9% (83/238) of expected opioid-down samples contained a benzodiazepine
- The most common benzodiazepine in opioid-down samples was bromazolam (73), followed by benzodiazepine (unknown type) (9), and desalkylgidazepam (2).
- Xylazine was detected in 8.8% (21/238) of opioid-down samples, most commonly being found in samples from Substance (15).
In October, 50.4% (120/238) of all opioid-down samples checked contained an additional active to the expected fentanyl/heroin. These data are shown in Fig. 3 highlighting the prevalence of benzos, fluorofentanyl, ortho-methyl fentanyl, and xylazine in the down supply.
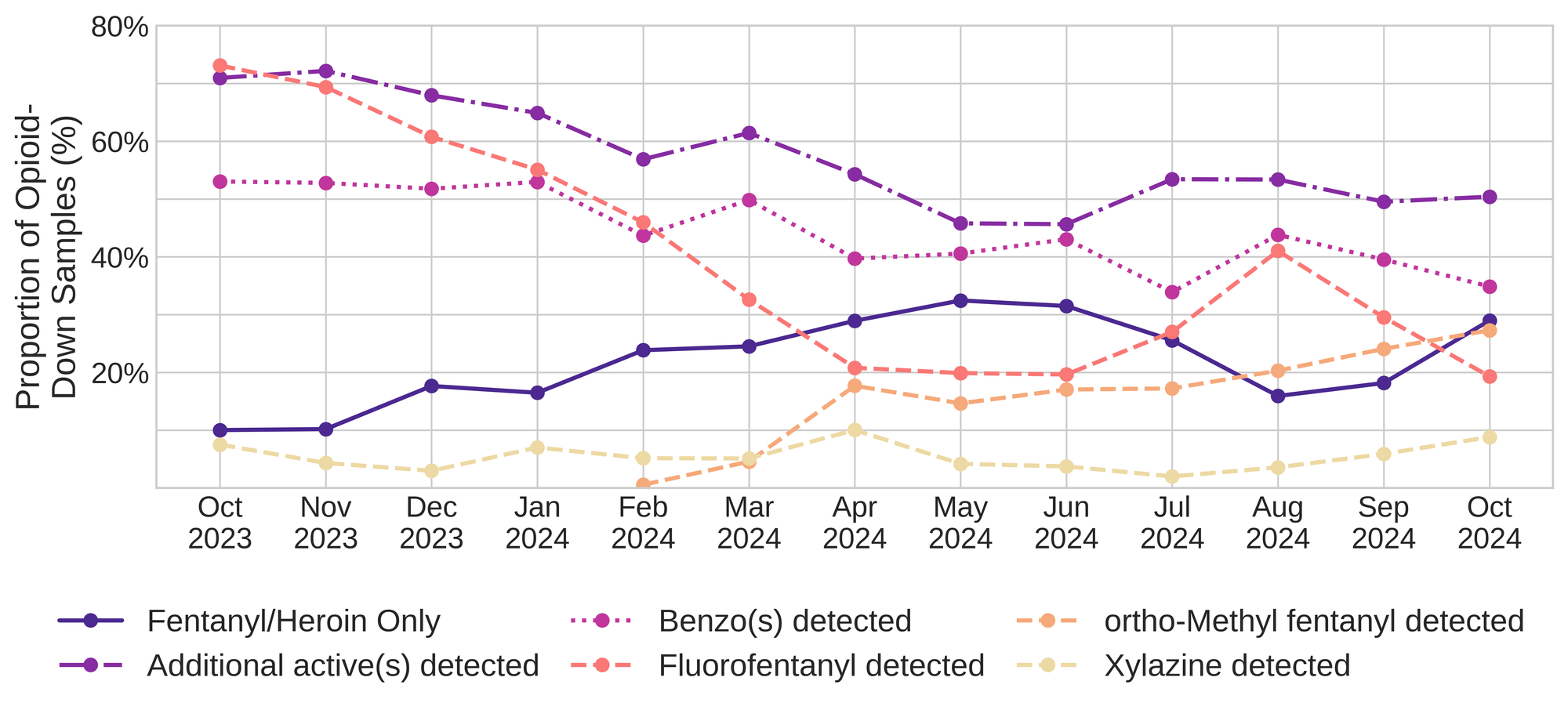
Ortho-Methyl fentanyl, a fentanyl analogue which appeared in Victoria's down supply at the start of 2024, was found in 27.3% (65/238) of opioid-down samples. This makes ortho-Methyl fentanyl the second most common additional active found within the opioid-down supply. Ortho-Methyl fentanyl is a fentanyl analogue that is thought to be similar in potency or slightly weaker than fentanyl, however, there are very few studies on its effect in humans.
Fluorofentanyl (specifically the HCl salt) was the thrid most common additional active found within the opioid-down supply, with 14.3% (34/238) of opioid-down samples containing fluorofentanyl in addition to other active compounds, including fentanyl. Additionally, fluorofentanyl was the only opioid detected in 5% (12/238) of opioid-down samples (i.e. no fentanyl or heroin was detected in these samples). Overall, 19.3% (46/238) of opioid-down samples contained fluorofentanyl.
Benzo-related drugs contribute to a majority of the other additional actives found in expected opioid-down samples, with 34.9% (83/238) of expected opioid-down samples checked containing a benzo-related drug. Bromazolam continues to be the most common benzo seen in the down supply, being detected in 88% (73/83) of the benzo-positive opioid-down samples. This makes it just slightly more common than ortho-methyl fentanyl within the opioid-down supply.
Scattered detections of other drugs are still found and can be reviewed in the pdf report at the end of this blog.
Quantification for Expected Opioid-Down[1]
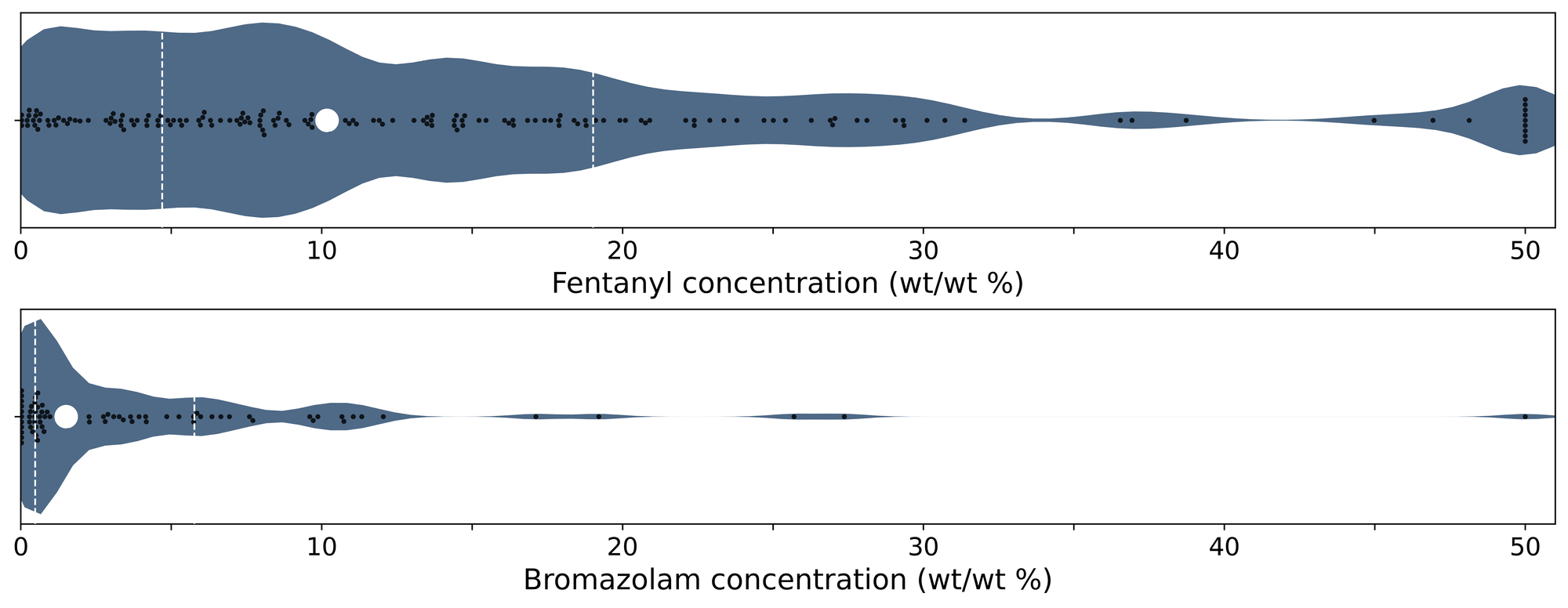
In October, we quantified fentanyl for 162 of the expected opioid-down samples containing fentanyl and found the median concentration to be 10.3%[2]. Though the median is a useful indicator, it doesn’t capture the volatility of fentanyl concentrations present in the opioid supply, as half of fentanyl-positive down samples contained between 5.1% and 19% fentanyl, and any one sample might be the lowest strength (less than 0.1%) or the strongest (greater than 50%[3]). Fluorofentanyl was seen at concentrations ranging from 0.2% to 28.5% as well, with a median concentration of 4.7%. In October, we quantified ortho-Methyl fentanyl in 60 opioid - down samples at a median concentration of 3.5%, with half of ortho- Methyl fentanyl positive down samples containing between 1.4% and 8.4% ortho-Methyl fentanyl. Bromazolam, the most common benzodiazepine adulterant in down samples, had concentrations ranging from less than 0.1% to greater than 27.4%[3:1] bromazolam, with a median of 2.5%. For context, a sample containing 4% bromazolam would be roughly equivalent to two full 2mg Xanax bars worth of benzo per point (100mg).
Not all opioid down samples brought to our service can be quantified. This is primarily due to too limited sample collected for our instruments to report a reliable mass percentage. Nevertheless, qualitative detection is still possible. ↩︎
This number is specific to fentanyl quantified in opioid-down samples. The median concentration listed in the Key Findings at the beginning of this blog (11%) is inclusive of all samples checked, across all drug classes and unknown samples, that contained fentanyl. ↩︎
For samples that contain greater than 50% fentanyl, heroin, fluorofentanyl, or bromazolam by weight, our mass spectrometer is presently unable to reproducibly assign a concentration due to the upper limits of the calibration methods currently adopted. ↩︎ ↩︎
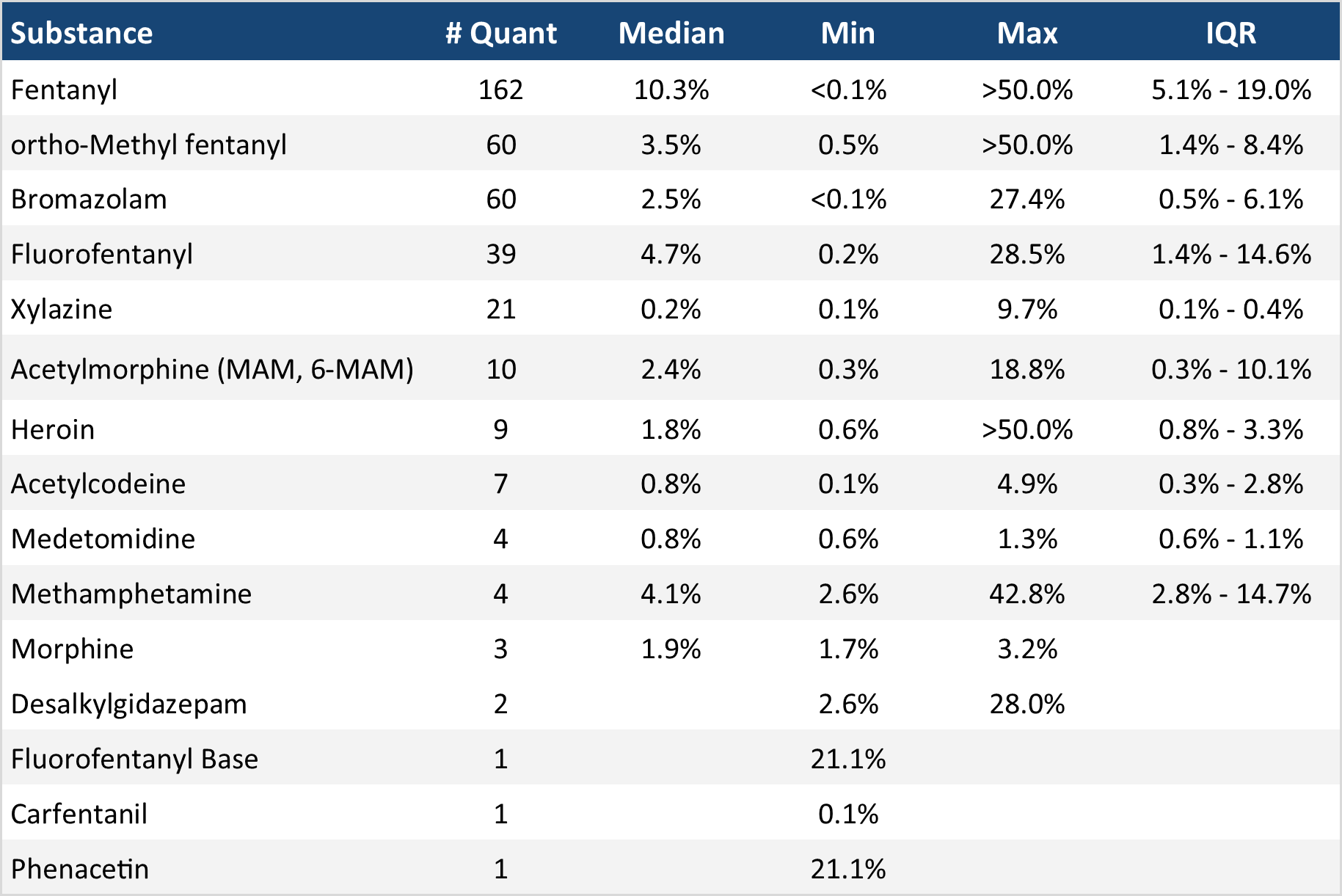
The fentanyl and bromazolam concentrations that we quantified in October, across all expected drug categories and service models, are presented in Fig. 4. Small black dots are individual opioid-down samples, the large white dot shows the median concentration, dashed white lines bound half of the quantified samples, and the width of the shaded regions mirrors the number of samples at a given concentration.
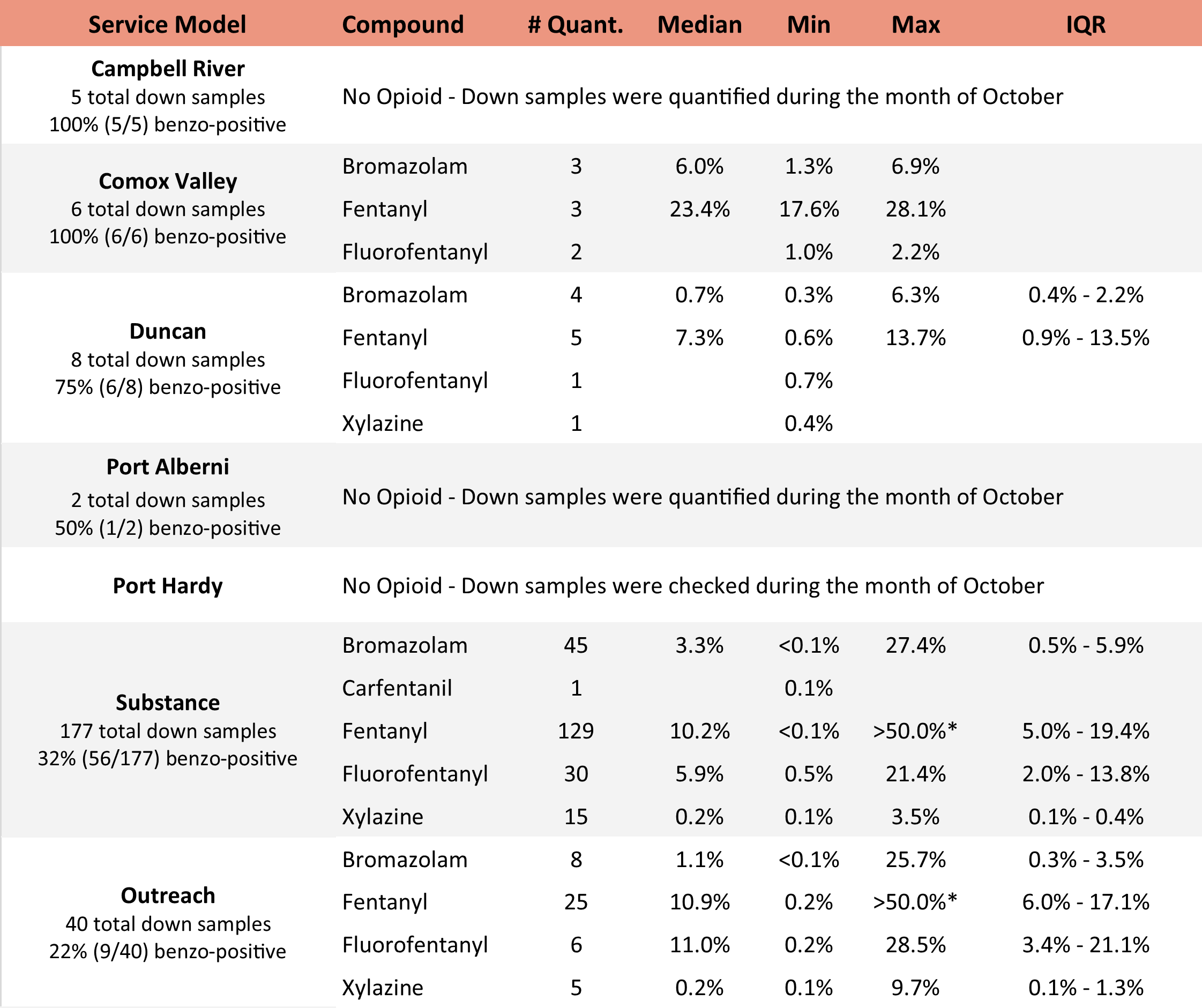
We can also examine the regional variability in the unregulated market. The table below expands on the quantitative data presented above. It focuses only on fentanyl, fluorofentanyl, carfentanil, bromazolam, and xylazine quantified within expected opioid-down samples, separated by collection location/model. Weight percentage is reported; “IQR” is the interquartile range: the range that contains half of the quantified samples.
Want to be notified when we release these reports? Join our mailing list by clicking the button below. You'll receive updates about when our reports are available directly in your inbox. You can subscribe and unsubscribe from this list at any time.
Check back next month for the November report!
As always, send us feedback at substance@uvic.ca on how we can continue to offer our drug checking results in a useful way.
