July 2023 Monthly Report

In this blog post, we discuss our July 2023 report and provide more information on how to interpret the results. The PDF report can be found at the end.
Key findings:
- The median fentanyl concentration found across all drug categories was 9.1%
- Carfentanil was found in 5 samples (4 expected opioid-down, 1 “unknown”) with a median concentration of 0.84% and maximum concentration of 8.76%, the highest concentration we have seen to date
- Benzodiazepines and/or etizolam were found in 50% (192/386) of expected opioid-down samples
- Bromazolam, the most common benzo found within opioid-down, was found in 159 opioid-down samples with a median concentration of 3.5% and maximum concentration of 26.4%
- Xylazine was found in 21 samples (all expected opioid-down) with a median concentration of 0.9% and a maximum concentration of 13.2%
Insight for the July 2023 Monthly Report
This blog, and the associated pdf report, breakdown our sample counts into six categories:
-
samples received through direct service provision in Victoria, where service users are bringing samples into the Substance storefront. These samples are labelled as “Substance” samples in the figures/tables of this blog post
-
samples received through direct service provision in Campbell River, where service users bring samples to the Vancouver Island Mental Health Society (VIHMS). These samples are labelled as “Campbell River”.
-
samples received through direct service provision in the Comox Valley, where service users are bringing samples to AVI Health & Community Services in Courtenay, BC. These samples are labelled as “Comox Valley”.
-
samples received through direct service provision in the Cowichan Valley, where service users bring samples to the Duncan Lookout Society OPS in Duncan, BC. These samples are labelled as “Duncan”.
-
samples received through direct service provision in Port Alberni, where service users bring samples into Port Alberni Shelter Society’s OPS. These samples are labelled as “Port Alberni”.
-
samples received through indirect service provision, where samples are collected through no-contact drop-off envelopes, are collected by harm reduction workers and other community members at supported housing sites, overdose prevention sites, and supervised consumption locations. These samples are labelled as “Outreach” samples in the figures/tables herein. July’s Outreach data includes samples collected at the Phillips Backyard Tilt! event series and at the Salt Spring Island Pride festival.
Drug types
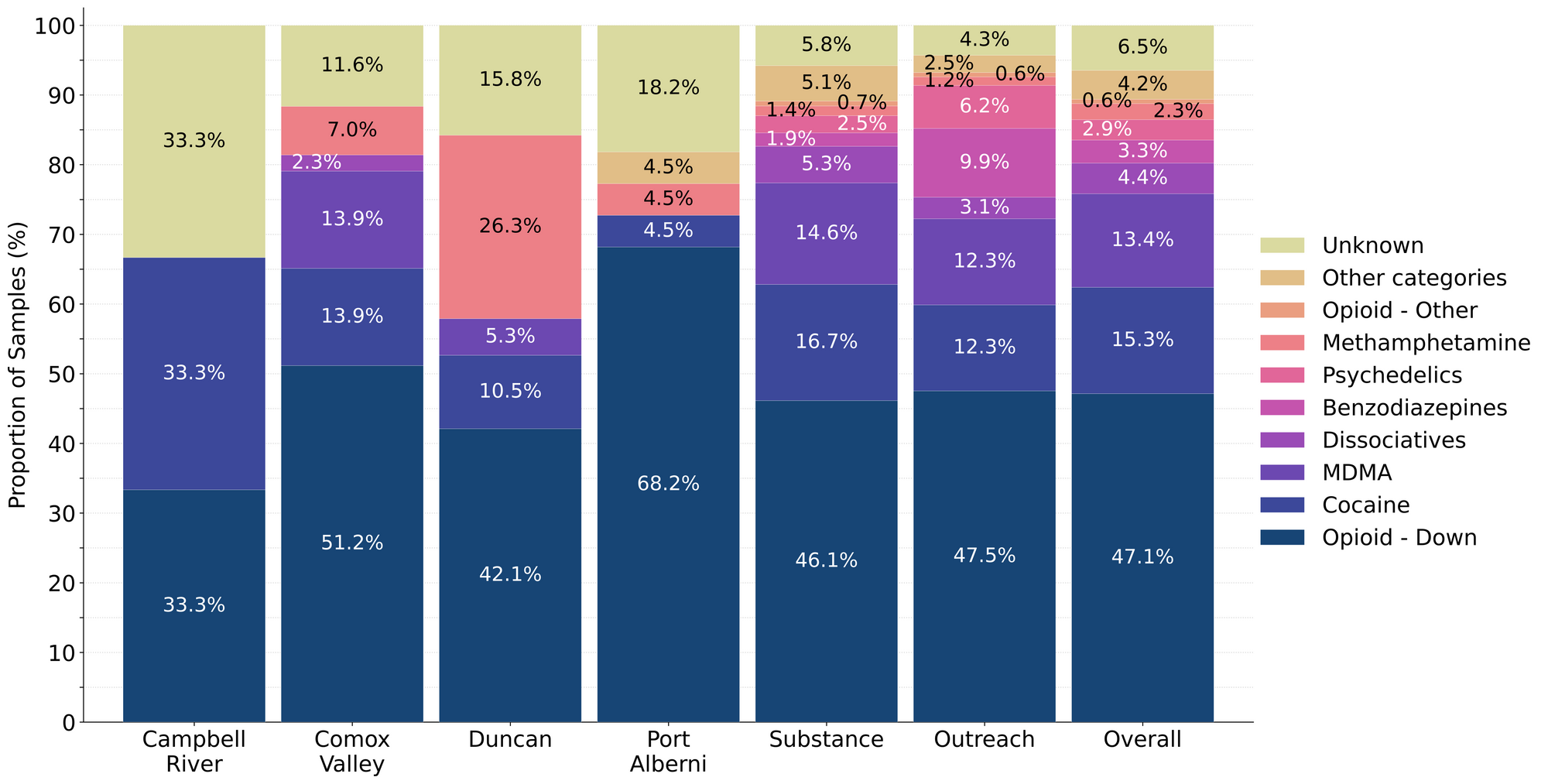
Fig. 1 shows the prevalence of each expected drug category checked, split by sample collection location/method.

Summer’s simple sample summary and the sketchy substance slushie scoop
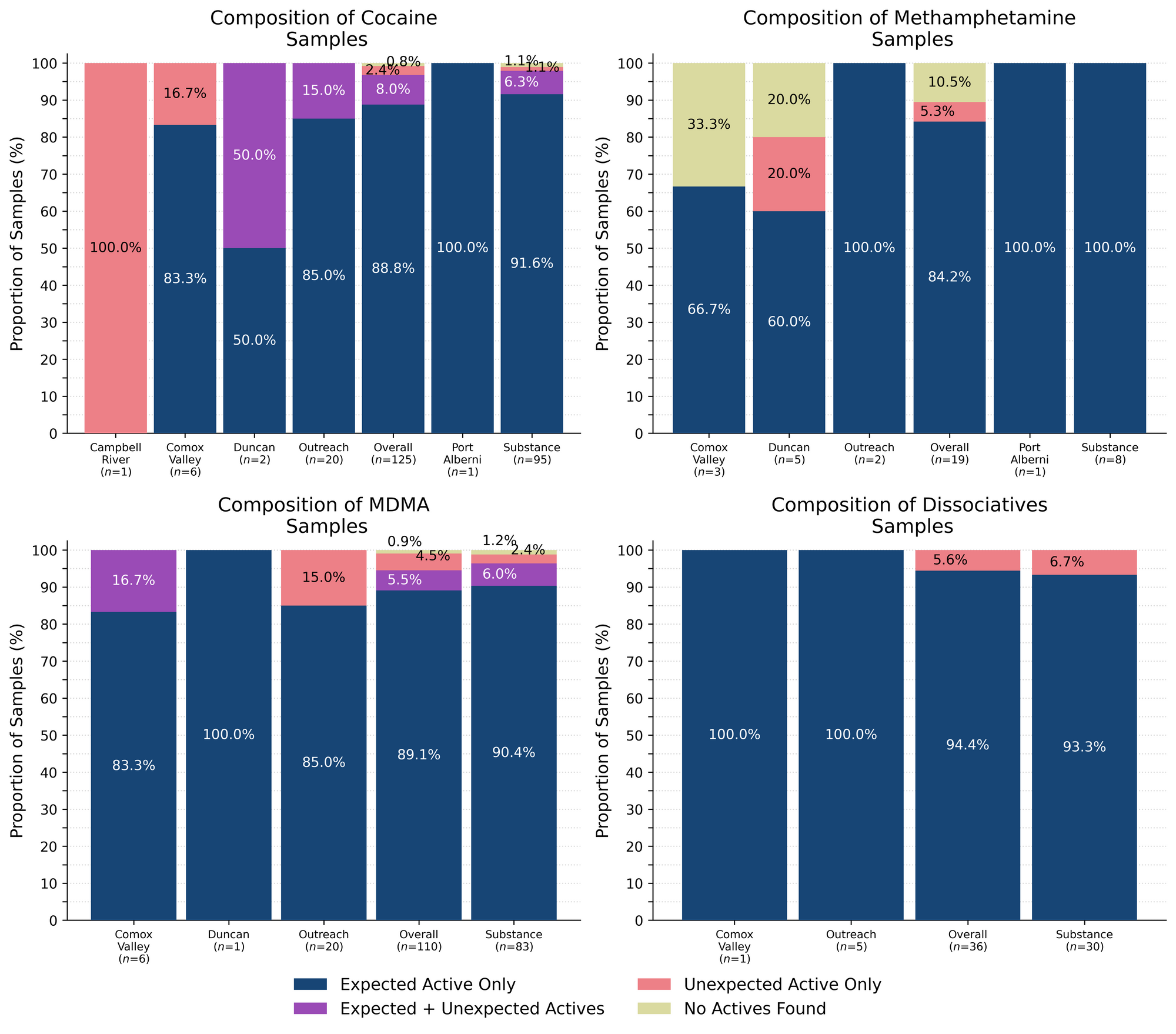
For the majority of samples checked, we confirm the presence of the expected drug with no additional active compounds detected above the limitations of the drug check. The bar charts below highlight a few classes of drugs, differentiating samples where only the expected active component was detected - from situations when other unexpected active components were detected.
94% (34/36) of expected ketamine samples checked in July were confirmed to be ketamine with no other active compounds detected.
Within the remaining two expected ketamine samples:
- One sample was found to contain Fluorexetamine (3'-Fluoro-2-oxo-PCE, FXE) instead of the expected ketamine. Fluorexetamine is a ketamine analog and would likely have similar effects, although research into the substance is lacking.
- One sample was found to be methamphetamine, instead of the expected ketamine
89% (111/125) of expected cocaine samples (90 cocaine HCl/soft, 21 cocaine base/hard/crack) were confirmed to be cocaine with no additional active compounds detected. Two of these samples were found to contain inactive cutting agents, with pyridoxine (Vitamin B6) detected in one sample at around 25%, and caffeine detected in another sample at roughly 50%. Both samples were from Victoria.
10 samples contained an active component in addition to cocaine:
- Benzocaine - One sample (Victoria); a topical local anaesthetic. This sample contained around 70% benzocaine
- Levamisole - Three samples (x1 Victoria, x2 Outreach); an antihelminthic drug used to treat parasitic worm infections, commonly seen as a cut in cocaine. Levamisole concentrations ranged from 0.2% to 6%
- Phenacetin - Five samples (x1 Duncan, x3 Victoria, x1 Outreach); “super buff” a tylenol-like drug, commonly seen as a cut in cocaine. Phenacetin concentrations ranged from around 0.3% to 65%
- Procaine - One sample (Victoria); a topical local anaesthetic. This sample contained around 7% procaine
The four remaining expected cocaine samples did not contain cocaine:
- Two samples were found to be ketamine; one was from the Comox Valley and the other from Victoria. Clumpy white powders in unlabeled baggies can be a head scratcher, so we are always eager to use our spectrometers to help you identify your sample before more qualitative experiments are run in your nose.
- One sample from Campbell River was found to be meth instead of cocaine. This sample was a clear crystalline rock that was reported to be “stronger than expected”.
- One sample from Victoria was found to just be sodium chloride; some people may be salty over these results.
89% (98/110) of expected MDA/MDMA samples checked were confirmed to be MDA (5 samples), MDMA (92 samples), and MDPM (1 sample) as expected. The remaining expected MDA/MDMA samples displayed a range of compositions, with the MDA-to-MDMA mixup representing a majority of the samples:
- Four expected MDA samples were found to be MDMA instead. Two samples were checked in Victoria and the other two through Outreach services.
- Four expected MDMA samples were found to be mixtures of both MDA and MDMA. All were checked in Victoria.
- Two expected MDMA samples were found to be a mixture of MDMA and MDEA. MDEA (MDE/“Eve”) is reported to be less potent and less stimulating than MDMA but generally produces similar effects. One sample was checked in the Comox Valley and the other in Victoria.
- One expected MDPM sample contained no MDPM and was found to be 4F-PHP instead. 4F-PHP is a novel substituted cathinone with extremely limited information available regarding dosage and effect. As always, and especially with novel substances, general harm reduction practices are encouraged.
84% (16/19) of expected methamphetamine samples checked were found to be meth with no other active compounds detected. Inactive cuts were detected in one (approximately 10%) of these samples, with caffeine detected in a meth sample from Victoria.
Of the remaining two expected methamphetamine samples:
- One sample from Duncan was found to contain sucrose, or table sugar. No other compounds were detected
- One sample from the Comox Valley, described as having a “styrofoam feel”, was found to not have any detectable compounds and may have simply been styrofoam.
Benzodiazepines (n=27)
85% (23/27) of the expected benzodiazepine samples checked in July came to our service sites in the form of pressed pills with the following expected and detected compositions:

Within the remaining four samples:
- One sample from Victoria was expected to be bromazolam and was confirmed to contain the expected benzo. This sample was described as a “fluffy cream” coloured powder, a possible allusion to the smooth hypnotic weightlessness experienced when floating through benzo-induced cloudspaces.
- Three samples were expected to be pyrazolam. One was confirmed to be pyrazolam, while the other two were found to be desalkylgidazepam and N-desalkylflurazepam instead. All three samples were checked in Victoria
Opioid-positivity in non-opioid-down samples
In July, we checked 380 samples that were not expected to contain fentanyl or other “unexpected” opioids[1]. Since the opioid-down supply is no longer “just heroin” or “just fentanyl” and is instead a complex, potent, and ever-changing polysubstance market containing other synthetic opioids like fluorofentanyl or nitazenes, here we will examine the prevalence of any unexpected opioid, not just fentanyl, detected in non-opioid-down samples.
Specifically, we are excluding samples that were expected to be “opioid-down” or samples that had an “unknown/missing” expected composition. In the case of “opioid-other” samples, e.g. hydromorphone tablets and oxycodone pills, “unexpected opioids” are defined as any opioid that is not the expected opioid. ↩︎

Examining Table 3, we find that only one sample tested positive for unexpected opioids in July, representing 0.3% of all non-opioid-down samples checked. This sample was an expected oxycodone pill that was found to contain metonitazene instead. This pill was a round light blue pill with "M30" pressed into one side.
In July, no unexpected opioids were detected in samples expected to be cocaine, MDMA, dissociatives, methamphetamine, or psychedelics.
In people’s personal quests for bodily autonomy and informed consumption, there is often evaluation of risk and consequence, but when the consequences can be severe and the risks are unknown or are intentionally exaggerated, these become difficult, if not impossible, conversations to weigh. We believe that drug checking can help provide people with the information needed to evaluate the risks, and provides harm reduction advice to minimize undesired consequences of substance use. These data are not meant to downplay concerns or invalidate past experiences. We recognize the tragic consequences of when fentanyl is found in non-opioid samples and honour the heartbreak that such experiences produce. Instead, we present these data with the intent to combat misinformation and provide an evidence-based context for people to consider when making decisions about substance use. While these numbers reflect what we have seen over the course of the project, these (roughly) 1-in-200 events still occur, so we always encourage folks to get their stuff checked.
Opioid-Down (n=386)
In this section we present results specific to the opioid-down supply, therefore they may differ from the highlighted findings above that are inclusive of all expected drug categories.
- 87% of expected opioid-down samples contained fentanyl (335/386)
- 20 samples contained heroin (5% of expected opioid-down samples)
- Seven samples were heroin (and related alkaloids like acetylmorphine (MAM) and acetylcodeine) with no other active compounds detected. Caffeine was found as a cut in two samples and erythritol (a sugar) in one sample. Five samples were mailed-in and the other two were checked in Victoria
- The other 13 samples contained heroin with the additional actives fentanyl, fluorofentanyl, carfentanil, bromazolam, etizolam, and lidocaine sporadically detected in various concentrations as well
- 53% of expected opioid-down samples contained fluorofentanyl (204/386)
- Four samples contained carfentanil (1% of all opioid-down samples)
- One sample from Victoria contained 8.76% carfentanil with caffeine as a cutting agent. This is the highest concentration of carfentanil seen by our project to-date
- Three samples were checked in Port Alberni and contained carfentanil ranging from 0.2% to 2.1% alongside fentanyl and benzodiazepines
- 50% of expected opioid-down samples contained a benzodiazepine and/or etizolam (192/386)
- Xylazine was detected in 6% (22/386) of opioid-down samples
In July, 67% (260/386) of all opioid-down samples checked contained an additional active to the expected fentanyl/heroin. These data are shown in Fig. 3 highlighting the prevalence of benzos, fluorofentanyl, and xylazine in the down supply.
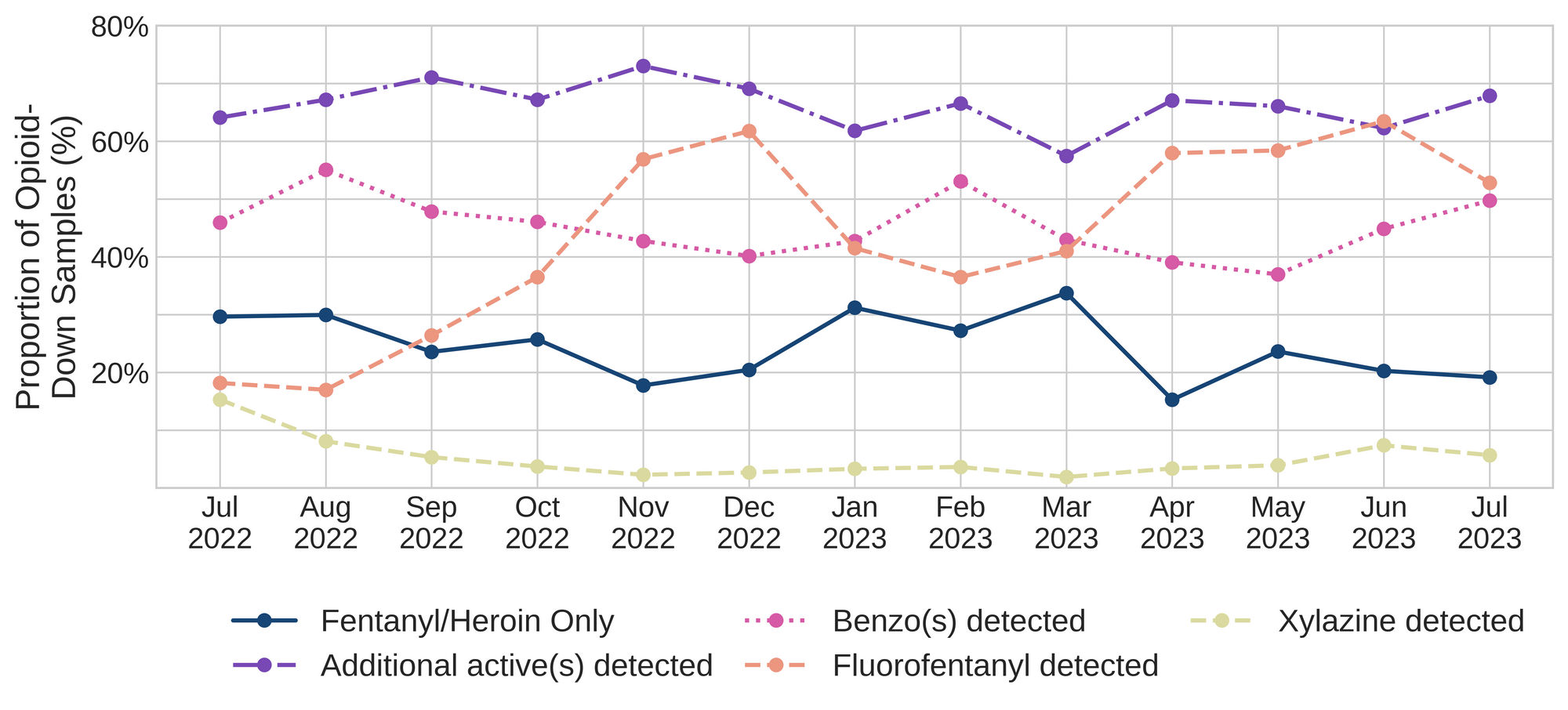
Fluorofentanyl was the most common additional active found within the opioid-down supply, with 43% (166/386) of opioid-down samples containing fluorofentanyl in addition to fentanyl. Additionally, fluorofentanyl was the only opioid detected in 13% (52/386) of opioid-down samples (i.e. no fentanyl or heroin was detected in these samples).
Benzo-related drugs contribute to a majority of the other additional actives found in expected opioid-down samples, with 50% (192/386) of expected opioid-down samples checked containing a benzo-related drug. Bromazolam continues to be the most common benzo seen in the down supply, with bromazolam being detected in 85% (160/188) of the benzo-positive opioid-down samples. Scattered detections of other drugs are still found and can be reviewed in the pdf report at the end of this blog.
Quantification for Expected Opioid-Down[1]
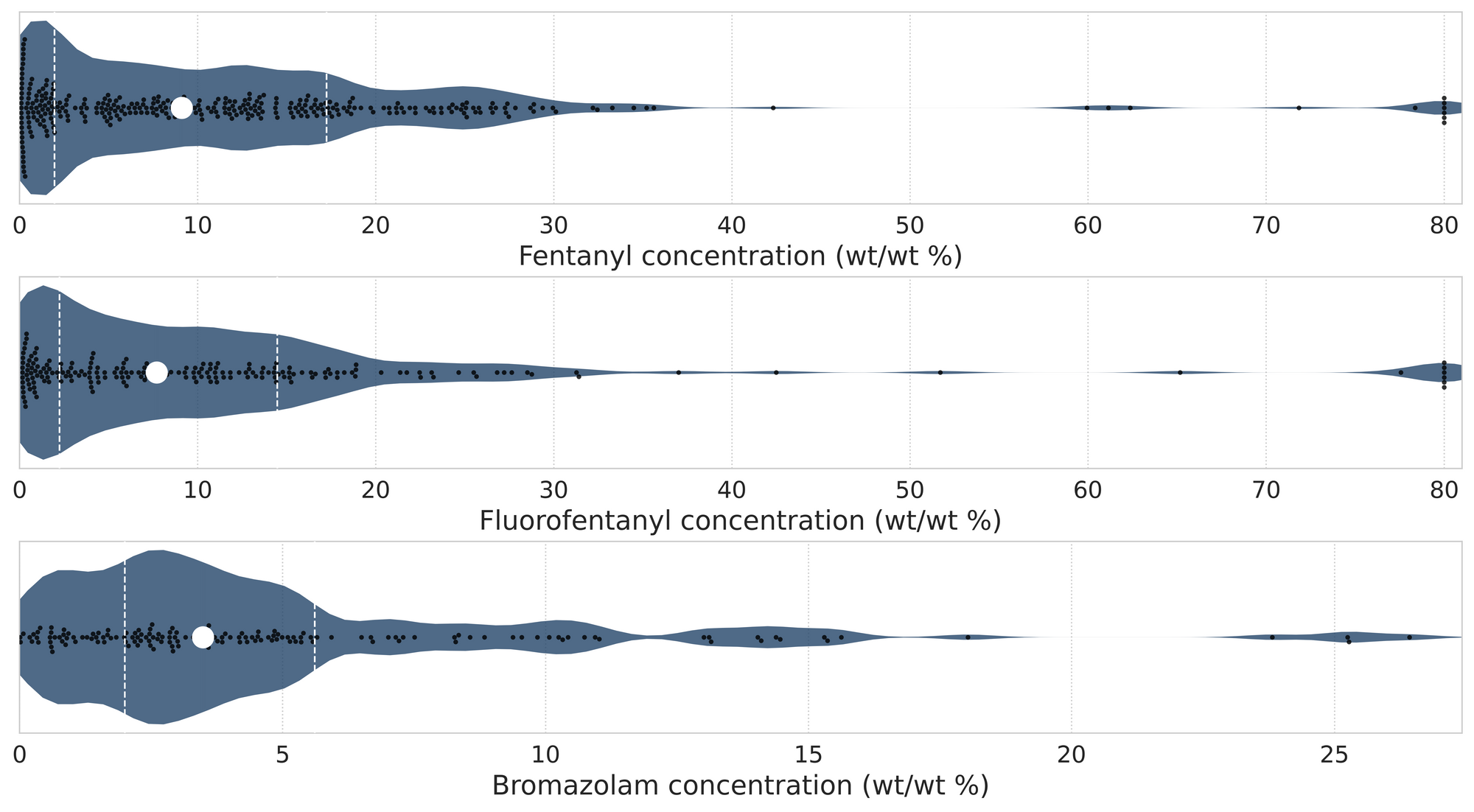
In July, we quantified fentanyl for 327 of the expected opioid-down samples containing fentanyl and found the median concentration to be 9.1%[2]. Though the median is a useful indicator, it doesn’t capture the volatility of fentanyl concentrations present in the opioid supply, as half of fentanyl-positive down samples contained between 2.0% and 17.2% fentanyl, and any one sample might be the lowest strength (0.1%) or the strongest (>80%[3]). Fluorofentanyl was seen at concentrations ranging from 0.2% to greater than 80% as well, with a median concentration of 7.7%. Similarly, the concentration of bromazolam was across the board in expected opioid down samples, with samples ranging from less than 0.1% to 26.4% bromazolam, with a median of 3.5%. For context, a sample containing 4% bromazolam would be roughly equivalent to two full 2mg Xanax bars worth of benzo per point (100mg).
Not all opioid down samples brought to our service can be quantified. This is primarily due to too limited sample collected for our instruments to report a reliable mass percentage. Nevertheless, qualitative detection is still possible. ↩︎
This number is specific to fentanyl quantified in opioid-down samples. The median concentration listed in the Key Findings at the beginning of this blog (also 9.1%) is inclusive of all samples checked, across all drug classes and unknown samples, that contained fentanyl. ↩︎
For samples that contain more than 80% fentanyl, or more than 25% etizolam by weight, our mass spectrometer is presently unable to reproducibly assign a concentration due to the upper limits of the calibration methods currently adopted. ↩︎

The fentanyl, fluorofentanyl, and bromazolam concentrations that we quantified in July, across all expected drug categories and service models, are presented in Fig. 4. Small black dots are individual opioid-down samples, the large white dot shows the median concentration, dashed white lines bound half of the quantified samples, and the width of the shaded regions mirrors the number of samples at a given concentration.
We can also examine the regional variability in the unregulated market. The table below expands on the quantitative data presented above. It focuses only on fentanyl, fluorofentanyl, carfentanil, bromazolam, and xylazine quantified within expected opioid-down samples, separated by collection location/model. Weight percentage is reported; “IQR” is the interquartile range: the range that contains half of the quantified samples.

Want to be notified when we release these reports? Join our mailing list to receive updates about when our reports are out. You can subscribe and unsubscribe yourself from this list at any time.
As always, send us feedback at substance@uvic.ca on how we can continue to offer our drug checking results in a useful way.
