Fentanyl Screening Is Not Drug Checking
Drug advisories that lack nuance and context, like the ones put out by Public Health, only serve to remind us of all the things governments could be doing but aren’t.
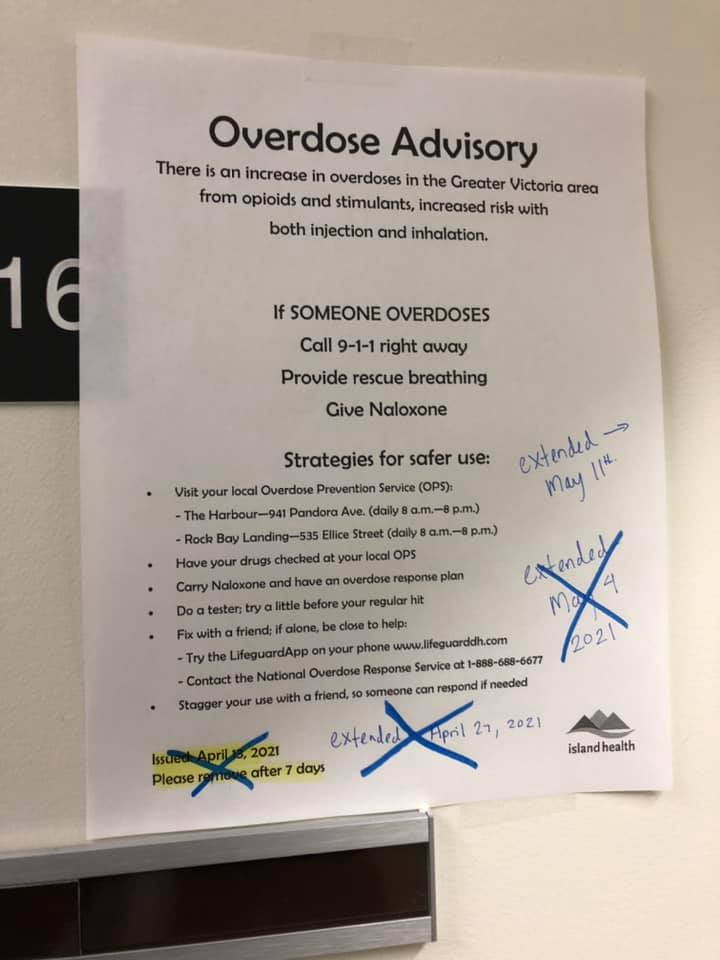
(Photo provided by Lorna Mace who writes that “this photo is posted on the door of my office and I refuse to continue to reprint the notifications. I want the world to see that every Tuesday I just come into work, check my email, and revise my sign.")
Recently, like so many times before in the ongoing overdose emergency, an Overdose Advisory was issued in our service region by Island Health, and then repeatedly extended. Overdose advisories and sometimes Drug Alerts are put out by Public Health and other agencies when an increase in overdose events occurs. In them, recommendations for reducing the risk of overdose are outlined; among which are directives not to use alone and to get drugs checked at local overdose prevention sites. These recommendations are important, but let’s be honest, in the context of prohibition, limited access to overdose prevention services and governments that have fought the provision of effective harm reduction for decades, they continue to be superficial attempts at reducing drug related harms. If anything, they remind us of the volatility and dangers of unregulated drug markets. This condition, far from being exceptional like the advisories suggest, is the everyday reality of an illicit drug market with little to no quality controls.
Drug alerts have been the source of critique among some harm reduction advocates for years. While some people point to drug alerts as a way to warn others of ‘bad batches,’ others have discussed their propensity to be alarmist and ineffective, exceptionalizing what is a consistent supply issue. Alert fatigue and the lack of utility for generic ‘white powder tested positive for fentanyl’ warnings only serve to contribute to a growing skepticism of the effectiveness of such warnings. Disagreements exist not only about whether to release alerts or not, but how to release them in ways that are useful, effective and reflective of the wishes of the community they aim to protect.
For example, DanceSafe, one of the pioneers of rave harm reduction who have been releasing alerts through their Test It! Alerts system, recently released a statement about why they use alerts. This statement was a response to ongoing discussions surrounding the use of alerts more broadly. In their statement, they point out that “Test It! Alerts are not intended to indicate that a certain form of a certain substance is one to “look out for;” rather, they should be internalized as a reminder of just how broad and unregulated the illicit drug market is, and how even an unassuming-looking substance can contain completely different chemicals than what it is marketed as to the consumer.” These alerts are done with the care needed to contextualize their use in the reality of unpredictable markets.
Unlike the alerts put out by Public Health and enforcement agencies, DanceSafe’s Test it! alerts come from a rich history of grassroots drug use and harm reduction within dance/rave communities where there is a strong sense of collective responsibility and already established trust. DanceSafe accurately points to the community relationships needed to make alerts more effective: “[s]haring alerts with others, either digitally or by word of mouth, with accompanying explanations of what they imply and how others should interpret them, spreads the message of the importance of harm reduction practices and helps make the general public more aware of how risky illicit purchases truly are. We can’t do this part without you.”
Alerts tend to work best when disseminated amongst the community from trusted information and sources. What makes DanceSafe’s alerts different from the advisories presented above is that DanceSafe is embedded within the community as an established, trusted and grassroots movement interested and dedicated to harm reduction in dance communities. Another example of such a relationship could be the Dope Guide in Victoria, BC, that was put out by local harm reduction organizations to provide a small snapshot into the available supply that included user experiences supplemented with drug checking data. Both examples suggest that community relations and established trust go far in providing effective information about local supplies. Unfortunately, this level of trust does not exist with government agencies that have fought harm reduction efforts for decades and who continue to put out advisories while offering little to change the conditions that create unstable and dangerous drug markets in the first place.
As mentioned, our experience shows that drug alerts and warnings are best disseminated through the community by trusted members and advocates. When people who know the market and community intimately disseminate information about the supply, it carries a weight not possible with public health advisories. Additionally, alerts put out by government agencies are reflected in the superficiality that exist in the messaging. In the context of criminalization and state violence towards people who use drugs, messages like “don’t use alone” are paradoxes void of the understanding that the current climate of criminalizing drug use already and effectively encourages people to use alone. When using in public can result in criminal prosecution, harassment, and police violence, using alone offers safety. Moreso, in a climate where discrimination and stigmatization of people who use drugs continue to exist, using alone is often the only option.
People use alone and have been using alone despite knowing the risks associated because government and non-profits have created the conditions that make using alone desirable and in many cases unavoidable. Pointing out the risks of using alone and encouraging use with others without addressing the issues that make using alone dangerous in the first place is just one of the reasons many people choose to skim past such prescriptions and advisories. Providing a safer supply, something government agencies actually have the jurisdiction to do, is much more effective in reducing overdose deaths than the constant and redundant advisories of the dangers of an illicit market; dangers already known and embodied by the people drug advisories aim to target.
While the language has changed from ‘not using alone’ to ‘using with someone,’ advisories disconnected from the communities they target continue to create distrust and distaste for those who deploy them. For example, in our Health region, these alerts point to overdose prevention services as a response to an unpredictable supply, but as the community knows well, overdose prevention services are severely lacking in both scale and scope in the region. Restrictive policies like barring doctoring (the practice of injecting for someone else), jugging (injecting in the jugular vein), or inhalation can impede people’s access to these life saving interventions. These barriers only serve to discourage the use of overdose prevention services.
It’s not just these policies that create barriers for access to overdose prevention services, but the fact that very few publicly accessible sites exist. In the Capital Regional District with a population of over 400,000 people, there are currently only two publicly available overdose prevention sites and both are in the City of Victoria. The other 12 municipalities in the CRD do not have these critical services. Across the Island Health region, few publicly available overdose prevention sites exist with limited capacity and coverage, this despite a public health emergency that’s been decimating communities for over five years.
Of final note, fentanyl screening is not drug checking. I repeat, fentanyl screening is not drug checking. Encouraging people to access an OPS to check their fentanyl for fentanyl is redundant. Despite advances in methodologies and technologies to chemically analyze illicit substances with greater accuracy, Public Health is still pointing to fentanyl test strips alone as drug checking. While fentanyl is the drug most associated with overdose deaths, it is an inconsistent, adulterated and unpredictable supply that continues to heighten risk. Fentanyl test strips can be useful for certain folks in certain settings, but the reality is that for a majority of cases, fentanyl screening without additional analysis isn’t very useful. This is especially the case for a supply where fentanyl is common and in many cases, desired. Offering drug checking that solely screens for fentanyl limits its utility to a few scenarios. This is why drug checking needs to be understood, and more importantly offered, beyond just fentanyl test strips.
The growing adulteration of benzodiazepines is showing how the illicit supply adapts and responds to restrictions and barriers. The emergence of fentanyl as the primary ingredient in heroin is just one example of such a process. Until we create the conditions for a safer and stable supply, and likely even after, drug checking services will be needed to provide quality control in a market that has little. Drug checking is not just about screening for fentanyl, it’s about confirming the presence or absence of substances, identifying misrepresentations, determining concentrations and so much more. While fentanyl test strips, and now benzodiazepine test strips, are important tools in drug checking, they are just one piece of the process.
Just as overdose prevention services are severely limited in the region, so too are comprehensive drug checking services. Currently, two projects exist on the Island. One offers 8 hours of coverage in Nanaimo, and the other offers 35 hours of coverage in Victoria. The rest of the region has nothing. Not only is drug checking lacking to a scale needed in the region, the current policy landscape stands in the way of increasing the expansion and reach of current projects. For example, a bar on transportation of substances to drug checking sites significantly limits the reach of such important services. This policy means outreach workers are prevented from supporting people and clients in accessing drug checking. While drug checking is being stated as a method to help in the current epidemic, simultaneous barriers sometimes prevent it from being a viable option. It doesn't make sense.
As the overdose crisis rages on, we’ll need to continue pushing governments to do better. Drug advisories that lack nuance and context, like the ones put out by Public Health, only serve to remind us of all the things governments could be doing, but aren’t. They simply remind us that the illicit market is constantly changing and morphing and will continue to do so. We don’t need more advisories from the very people who can make these advisories moot. People who use drugs already know that prohibition is deadly. What we really need is Public Health to massively scale-up harm reduction services, including drug checking; to work towards an end to criminalization; and importantly, to provide equitable and free access to an alternative, relevant, and safer supply of drugs. Anything less is unacceptable.

